In the realm of medical billing and coding, understanding the correct Current Procedural Terminology (CPT) codes is crucial for accurate documentation and reimbursement. One common procedure that often raises questions is suture removal. This article will delve into the specifics of the CPT code for suture removal, its importance, and related coding practices.
1) What is a CPT Code?
CPT codes are standardized numerical codes used by healthcare professionals to describe medical, surgical, and diagnostic services. Developed by the American Medical Association (AMA), these codes ensure uniformity in reporting and help streamline the billing process.
2) The Specific CPT Code for Suture Removal
Interestingly, there is no specific CPT code dedicated solely to the removal of sutures. This is because suture removal is typically considered part of the postoperative care of the initial procedure and is often included in the global surgical package. The global surgical package encompasses all necessary services normally furnished by a surgeon before, during, and after a procedure.
3) How to Code for Suture Removal
Since there’s no dedicated CPT code for suture removal, the coding depends on the context and timing of the removal:
- Postoperative Period: If the suture removal occurs within the global period of the surgical procedure, it is included in the postoperative care, and no separate code is billed.
- Outside the Global Period: If the removal occurs outside the global period, or the removal is done by a different physician who did not perform the original procedure, then you might use an Evaluation and Management (E/M) code. Commonly used E/M codes for such scenarios include 99211, 99212, or 99213, depending on the complexity of the service provided.
4) Detailed Explanation of E/M Codes
- 99211: This code represents a minimal service, usually involving a simple visit for a procedure like suture removal, requiring no physician’s presence.
- 99212: This code indicates a problem-focused visit, where a low level of medical decision-making is involved.
- 99213: This code is used for an expanded problem-focused visit, typically involving a more detailed history and examination.
5) When to Use Specific Codes
- Initial Procedure’s Global Period: No additional code is required as suture removal is bundled in the initial surgery’s global fee.
- Different Physician or Facility: If a different physician performs the suture removal or it occurs in a different facility, and the initial surgery was done by another provider, an appropriate E/M code may be billed.
- Beyond Global Period: If suture removal is required after the postoperative global period, use an appropriate E/M code based on the level of service provided.
6) Importance of Proper Coding for Suture Removal
Proper coding is crucial for several reasons:
- Accurate Reimbursement: Correct coding ensures that healthcare providers are appropriately compensated for the services they provide.
- Compliance: Adhering to coding standards helps avoid legal and financial repercussions associated with improper billing practices.
- Efficient Practice Management: Streamlined coding and billing processes lead to more efficient practice management and less administrative burden.
7) Scenarios Impacting Suture Removal Coding
- Emergency Room: If suture removal is performed in the emergency room (ER), it may be included in the ER visit code.
- Follow-Up Visit: During a follow-up visit, if suture removal is performed, it might be included in the follow-up visit code, especially if it’s part of postoperative care.
- Primary Care: If a primary care physician (PCP) removes sutures from a surgery performed by a specialist, the PCP might use an E/M code for the visit.
8) Documentation Tips for Suture Removal
Accurate and detailed documentation is essential for correct coding and reimbursement. Key points to include are:
- Date of Surgery: Document the date of the initial surgery to determine if the removal falls within the global period.
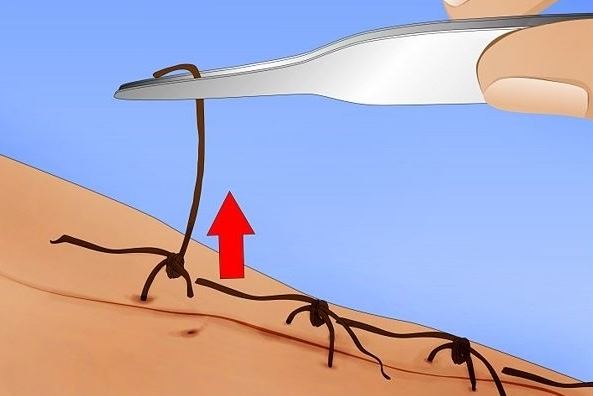
- Procedure Details: Clearly describe the suture removal process, including the number of sutures removed and the condition of the wound.
- Patient Information: Include relevant patient history and any complications or issues that necessitated the removal.
9) Case Studies
- Case Study 1: A patient returns to their surgeon 10 days postoperatively for suture removal. Since this visit falls within the global period, no additional CPT code is billed for the suture removal.
- Case Study 2: A patient visits their primary care physician three months after surgery for suture removal. The initial surgery was performed by a different surgeon. The PCP uses CPT code 99212 to bill for the suture removal, reflecting a problem-focused visit with low complexity.
- Case Study 3: A patient goes to an urgent care clinic for suture removal, and the initial surgery was performed by a different provider. The urgent care clinic bills using CPT code 99211, reflecting a minimal service visit.
Conclusion
Understanding the intricacies of CPT coding for suture removal is essential for healthcare providers to ensure accurate billing and reimbursement. While suture removal itself does not have a specific CPT code, the context and timing of the removal determine the appropriate coding practice. By adhering to proper coding guidelines and maintaining detailed documentation, healthcare providers can ensure compliance and optimize their practice management.