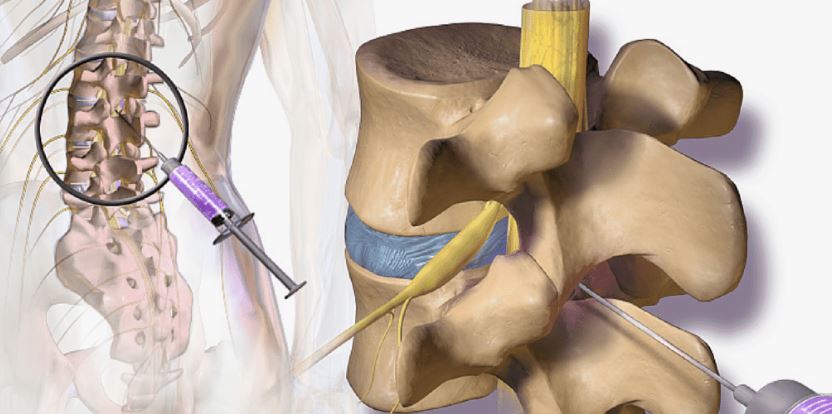
In the realm of pain management, X-ray guided facet injections have become an essential procedure for alleviating chronic pain, particularly in the spine. These injections target the facet joints, which are small stabilizing joints located between and behind adjacent vertebrae. While the medical benefits are significant, understanding the billing process for these procedures can be complex. This guide aims to demystify the billing process for X-ray guided facet injections, providing clarity for healthcare providers and billing specialists alike.
What is an X-ray Guided Facet Injection?
An X-ray guided facet injection involves the use of fluoroscopy (a type of X-ray) to ensure precise placement of the needle into the facet joint. The injection typically contains a combination of a local anesthetic and a corticosteroid to reduce inflammation and provide pain relief. This procedure is often used to diagnose or treat pain originating from the facet joints in the spine.
Importance of Accurate Billing
Accurate billing for X-ray guided facet injections is crucial for several reasons. It ensures proper reimbursement, avoids claim denials, and maintains compliance with healthcare regulations. Given the complexity of the procedure and the involvement of imaging guidance, detailed documentation and correct coding are paramount.
Key Components of the Billing Process
1. Patient Evaluation and Documentation
Before the procedure, a thorough evaluation of the patient is necessary. Documenting the patient’s medical history, symptoms, previous treatments, and the rationale for the facet injection is critical. Detailed documentation supports the medical necessity of the procedure and is essential for insurance claims.
2. Correct Coding
Coding for X-ray guided facet injections involves several components. The primary CPT (Current Procedural Terminology) codes used are:
- CPT 64490: Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), cervical or thoracic; single level
- CPT 64491: Injection(s), cervical or thoracic, second level (List separately in addition to code for primary procedure)
- CPT 64492: Injection(s), cervical or thoracic, third and any additional level(s) (List separately in addition to code for primary procedure)
- CPT 64493: Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral; single level
- CPT 64494: Injection(s), lumbar or sacral, second level (List separately in addition to code for primary procedure)
- CPT 64495: Injection(s), lumbar or sacral, third and any additional level(s) (List separately in addition to code for primary procedure)
3. Modifiers
Modifiers provide additional information about the procedure. Commonly used modifiers for facet injections include:
- Modifier 50: Bilateral procedure
- Modifier 59: Distinct procedural service
- Modifier LT/RT: Left side/right side
Using the correct modifiers ensures that the billing accurately reflects the services provided and avoids potential claim denials.
4. Image Guidance Documentation
Since the procedure involves image guidance, it’s essential to document the use of fluoroscopy or CT. This documentation should include details such as the type of imaging used, the reason for its use, and a description of the findings.
5. Medical Necessity
Demonstrating medical necessity is crucial for reimbursement. The documentation should include a detailed account of the patient’s condition, the reason for the facet injection, and the expected outcome. Insurance companies often require this information to justify the procedure.
6. Preauthorization
Many insurance companies require preauthorization for X-ray guided facet injections. This process involves submitting detailed information about the patient’s condition, previous treatments, and the proposed procedure. Obtaining preauthorization helps ensure that the procedure will be covered and reduces the risk of claim denials.
7. Claim Submission
Once the procedure is completed and documented, the claim must be submitted to the insurance company. The claim should include:
- Patient information
- Procedure codes
- Modifiers
- Documentation of medical necessity
- Image guidance details
8. Follow-Up and Appeals
If a claim is denied, it’s important to follow up promptly. Review the denial reason, correct any errors, and provide additional documentation if necessary. If needed, an appeal can be filed with the insurance company, presenting a detailed case for why the procedure should be covered.
Common Billing Challenges
1. Incorrect Coding
Using incorrect or incomplete codes can lead to claim denials. It’s crucial to stay updated with the latest CPT codes and ensure accurate coding for each procedure.
2. Insufficient Documentation
Lack of detailed documentation can result in denied claims. Ensure that all aspects of the procedure, including the use of image guidance, are thoroughly documented.
3. Preauthorization Issues
Failing to obtain preauthorization or providing insufficient information can lead to claim denials. Always check the requirements of the patient’s insurance plan and obtain preauthorization when necessary.
4. Modifier Misuse
Incorrect use of modifiers can cause billing errors. Ensure that the correct modifiers are applied based on the specifics of the procedure.
Best Practices for Successful Billing
- Regular Training: Ensure that billing staff receive regular training on the latest coding and billing practices.
- Thorough Documentation: Emphasize the importance of detailed documentation for every procedure.
- Preauthorization: Always obtain preauthorization when required and provide complete information.
- Audits: Conduct regular audits of billing practices to identify and correct any issues.
- Stay Updated: Keep abreast of changes in billing codes, insurance requirements, and regulatory guidelines.
Conclusion
X-ray guided facet injections play a crucial role in pain management, and accurate billing for these procedures is essential for healthcare providers. By understanding the key components of the billing process, utilizing correct coding and modifiers, ensuring thorough documentation, and obtaining necessary preauthorizations, providers can navigate the complexities of billing and ensure proper reimbursement. Regular training, audits, and staying updated with industry changes are vital practices for successful billing. With these strategies, healthcare providers can focus on delivering quality care while maintaining financial health.